Plantar fasciitis, also called Jogger’s Heel, is a widespread and often debilitating foot condition, that affects millions across the United States. Many individuals suffering from persistent heel pain seek effective solutions to regain their mobility and daily comfort. The stabbing pain that seems to intensify with each stride becomes an unwelcome companion for those living with plantar fasciitis. Delve into a groundbreaking alternative—Platelet-Rich Plasma (PRP) therapy. Discover how PRP offers a non-surgical lifeline for those desperately seeking relief from the relentless discomfort of Jogger’s Heel, offering a beacon of hope for individuals yearning to escape the constraints of their daily discomfort.

Understanding Jogger’s Heel
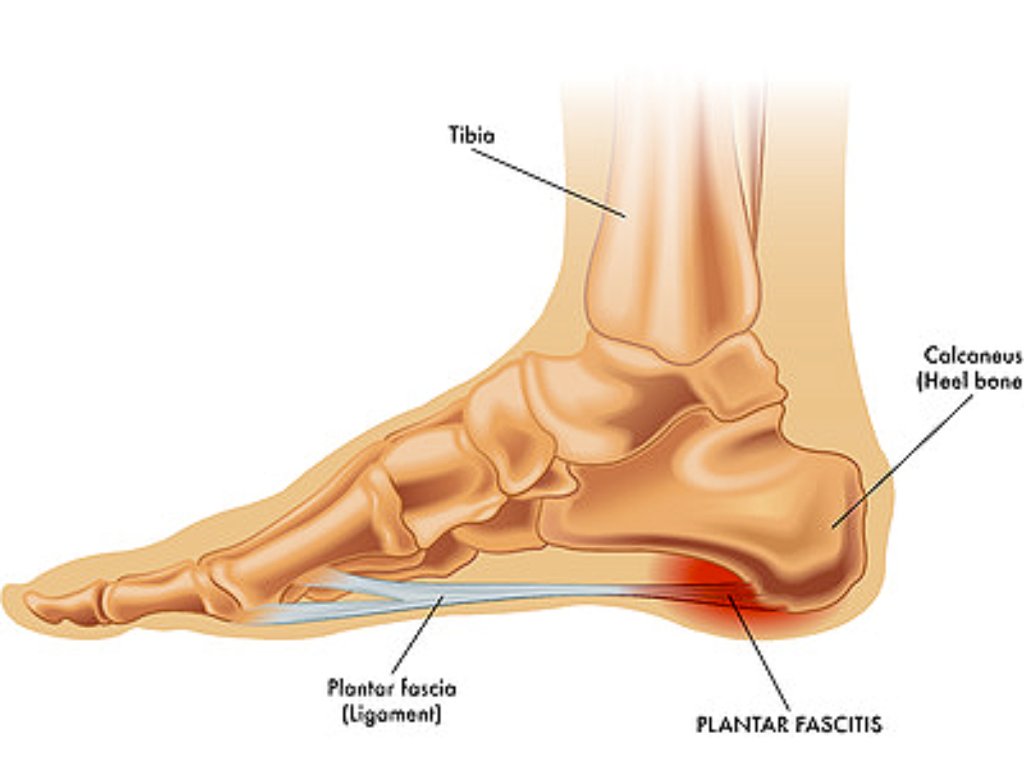
To comprehend the significance of PRP therapy, it’s essential to first understand the intricacies of plantar fasciitis. This common foot ailment arises from inflammation of the thick band of tissue connecting the heel bone to the toes, causing stabbing pain with every step.
The root causes, ranging from overuse to inadequate foot support, produce symptoms that can significantly impact an individual’s daily life. Conventional treatments, such as rest, ice, and anti-inflammatory medications, often provide only temporary relief.
As many people navigate through the challenges posed by conventional approaches, the pressing need for alternative solutions becomes evident. This sets the stage for the emergence of PRP therapy as a promising avenue for long-lasting relief.
Jogger’s Heel Symptoms and Causes
Plantar Fasciitis Symptoms:
- Intense heel pain: Individuals often experience a sharp and intense pain at the bottom of the heel when they take their first steps in the morning.
- Sharp pain at the bottom of the foot near the heel: The pain associated with plantar fasciitis is typically concentrated at the underside of the foot, specifically near the heel. This sharp pain can be felt along the length of the plantar fascia
- Increased discomfort after prolonged periods of standing or sitting: Whether it’s a long day on your feet or extended sedentary activities, the plantar fascia can become more strained, leading to an increase in pain and discomfort.
- Tenderness and inflammation in the heel area: Tenderness is a common symptom, and the affected heel may be sensitive to touch. Inflammation in the heel area may contribute to swelling, making the region around the plantar fascia appear red and feel warm to the touch.
- Difficulty in flexing the foot: Tightness and discomfort in the plantar fascia may result in difficulty flexing the foot, particularly when trying to point the toes upward. This restriction in movement can be a noticeable indicator of the impact of plantar fasciitis on foot flexibility.
Plantar Fasciitis Causes:
- Overuse or excessive strain on the feet: Common among athletes or those on their feet for extended periods
- Poor foot mechanics: Anatomical differences in feet such as flat feet or high arches
- Obesity or sudden weight gain: This can increase pressure and irritation on the feet
- Wearing improper footwear: Footwear with inadequate arch support, too tight, or too big. It is important to have properly fitting shoes.
- Tight Achilles tendons or calf muscles: This contributes to increased stress and strain on the plantar fascia, the thick band of tissue that connects the heel bone to the toes.
Understanding and addressing these contributing factors are essential for effective prevention and treatment.
Onset and Progression of Plantar Fasciitis
What are the Warning Signs of Plantar Fasciitis?
Gradual Onset: Plantar fasciitis often develops gradually over time. Many individuals may not recall a specific injury or event that triggered the condition.
Morning Pain: The hallmark symptom is intense heel pain, especially with the first steps in the morning. The pain can also be noticeable after prolonged periods of rest or inactivity.
Increased Activity Discomfort: As the condition progresses, individuals may experience heightened discomfort after prolonged periods of standing, walking, or engaging in activities that put strain on the feet.
Progression of Symptoms:
Persistent Pain: The pain associated with plantar fasciitis tends to persist and may evolve into a constant ache rather than a sharp sensation. It often radiates along the bottom of the foot, particularly near the heel.
Exacerbation After Activity: Physical activities, especially those involving weight-bearing on the feet, can exacerbate the symptoms. Pain may intensify during or after activities such as running, walking, or even climbing stairs.
Tenderness and Inflammation: Tenderness and inflammation may develop in the affected heel, making it sensitive to touch. Swelling may occur as a result of the ongoing stress on the plantar fascia.
Chronic Discomfort: Without intervention or proper treatment, plantar fasciitis can become a chronic condition. The persistent strain on the plantar fascia may lead to the development of heel spurs in some cases.
It’s crucial to note that the progression of Jogger’s Heel can be influenced by various factors, including the individual’s activity level, footwear choices, and underlying health conditions. Early recognition and intervention play a key role in managing symptoms and preventing the condition from becoming chronic. Individuals experiencing persistent heel pain should seek professional medical advice for an accurate diagnosis and tailored treatment plan.
Traditional Treatment Options for Jogger’s Heel
- Rest: Allow the inflamed plantar fascia to heal by avoiding activities that worsen symptoms.
Stretching Exercises: Improve flexibility and reduce tension on the foot by incorporating specific stretches for the calf muscles, Achilles tendon, and plantar fascia.
- Orthotic Inserts: Provide additional support and cushioning through custom or over-the-counter shoe inserts to distribute pressure more evenly and reduce strain on the plantar fascia.
- Supportive Footwear: Wear shoes with proper arch support, cushioning, and a supportive heel counter to alleviate stress on the plantar fascia during daily activities.
- Physical Therapy: Work with a physical therapist to develop a personalized exercise program that strengthens foot and leg muscles, improves flexibility, and corrects biomechanical issues contributing to plantar fasciitis.
PRP as an Alternative Treatment Option
As effective as traditional treatments can be, some individuals may seek alternative options for managing plantar fasciitis, particularly when conventional approaches yield limited results. One promising alternative gaining attention is Platelet-Rich Plasma (PRP) therapy. PRP involves extracting a concentrated form of the patient’s own blood, rich in platelets and growth factors, and injecting it into the affected area. This emerging treatment aims to stimulate tissue regeneration and accelerate the healing process.
How PRP Injections Work
At the heart of PRP therapy lies a natural and regenerative approach to healing. Platelet-Rich Plasma is a concentration of platelets derived from the patient’s blood, rich in growth factors that play a pivotal role in tissue repair and regeneration. The preparation process involves extracting a small amount of blood, processing it to isolate the platelets, and then injecting the PRP directly into the affected area.
By understanding the science behind PRP, individuals can appreciate its potential to address the root cause of plantar fasciitis. The concentrated growth factors within PRP stimulate the body’s natural healing processes, promoting the regeneration of damaged tissues and fostering a more robust and resilient foot structure.
The PRP Treatment Process
Embarking on the PRP therapy journey involves a series of well-defined steps, beginning with the initial consultation and assessment. During this phase, healthcare professionals evaluate the extent of the plantar fasciitis and determine the suitability of the individual for PRP treatment. Once the decision is made to proceed with PRP therapy, the patient undergoes a minimally invasive procedure where the Platelet Rich Plasma is precisely injected into the affected area.

What does a PRP appointment look like?
- Purpose: The core of the PRP therapy appointment involves a minimally invasive procedure designed to deliver the Platelet-Rich Plasma precisely to the affected area.
- Preparation: Before the injection, the healthcare professional may cleanse and numb the area to enhance patient comfort.
- PRP Extraction: A small amount of the patient’s blood is drawn, typically from the arm, and processed to isolate the Platelet-Rich Plasma.
- Precise Injection: Using advanced imaging guidance or palpation, the healthcare professional precisely injects the concentrated PRP into the targeted region. This ensures accurate placement for optimal therapeutic impact.
- Post-Procedure Guidance: After the injection, patients receive post-procedure guidance to enhance the effectiveness of PRP therapy and promote a smooth recovery.
- Activity Recommendations: Patients may receive advice on activities to avoid, optimal footwear, and any recommended exercises to support healing. While recovery experiences can vary, many individuals may resume normal activities with minimal downtime.
- Follow-Up: The healthcare team schedules follow-up appointments to monitor progress, address any concerns, and adjust the treatment plan if necessary.
- Natural Healing: PRP harnesses the body’s natural healing processes by utilizing concentrated growth factors from the patient’s blood. This promotes tissue repair and regeneration.
Advantages of PRP for Jogger’s Heal
One of the most compelling aspects of PRP therapy is its non-surgical nature. For individuals hesitant about undergoing invasive procedures, PRP offers a welcome alternative that harnesses the body’s natural healing mechanisms. The natural healing properties of PRP contribute to potential long-term relief and help a provider address the root cause of plantar fasciitis.
PRP therapy aims to not only alleviate symptoms but also promote lasting improvements in joint function, allowing individuals to regain mobility and engage in activities without the hindrance of chronic foot pain (1).
Main Advantages of PRP
- Minimally Invasive: As a non-surgical treatment, PRP therapy avoids the need for invasive procedures, providing a less intimidating and more comfortable option for individuals seeking relief.
- Reduced Downtime: Compared to traditional treatments, PRP therapy often involves minimal downtime, allowing individuals to resume normal activities more quickly after the procedure.
- Faster Recovery: The regenerative properties of PRP contribute to accelerated healing, potentially leading to faster recovery from plantar fasciitis compared to conventional methods.
- Minimal Side Effects: With PRP being derived from the patient’s own blood, the risk of adverse reactions is minimized, enhancing the safety profile of this regenerative treatment (2).
Seeking Professional Advice
While PRP Injections show promise, it’s crucial to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan. Specialized physicians can assess the severity of the condition and guide individuals in making informed decisions about their treatment options.
Conclusion
In conclusion, the key benefit of PRP for Jogger’s Heel is its appeal as a natural and effective treatment option. PRP stands as a beacon of hope to revolutionize the landscape of foot ailment management. Shedding light on these advantages encourages those contemplating regenerative medicine to explore its potential as a viable solution. The commitment to instilling confidence in individuals seeking lasting relief from chronic foot pain is a cornerstone of the advocacy for PRP therapy. This transformative journey is not just about alleviating symptoms, but encompasses a broader vision. The vision is to optimize joint health and enhance overall well-being. In closing, with the transformative potential of PRP, a future where individuals can reclaim their mobility, engage in daily activities without constraints, and enjoy life free from foot pain becomes a reality.
FAQ For Jogger’s Heel
Will Jogger’s Heel Go Away on Its Own?
Plantar fasciitis may resolve on its own with proper care and time. Rest, stretching exercises, and supportive footwear can alleviate symptoms, allowing the inflamed plantar fascia to heal. However, persistent cases may require more targeted interventions. Early and consistent application of appropriate treatments increases the likelihood of a natural recovery. However, individuals experiencing prolonged or severe symptoms should consult a healthcare professional for tailored advice and potential medical interventions.
What Shoes Should You Not Wear With Jogger’s Heel?
Individuals with plantar fasciitis should avoid shoes with inadequate arch support, minimal cushioning, or insufficient shock absorption. High heels and flat shoes provide inadequate support and can exacerbate symptoms. Tight or narrow footwear may also contribute to discomfort. It’s crucial to opt for shoes specifically designed for arch support, stability, and cushioning. Choosing footwear with proper features aids in relieving pressure on the plantar fascia. It also promotes a more comfortable and supportive environment
Is Running Good For Jogger’s Heel?
Running can be problematic for individuals with plantar fasciitis as it places repetitive stress on the foot. Impact and strain may exacerbate inflammation and pain. Some individuals find relief through proper footwear, gradual intensity, and stretching. Others may need to consider low-impact alternatives like swimming or cycling. It’s essential to listen to the body, modify activity as needed, and consult with a healthcare professional for personalized guidance while maintaining an active lifestyle.
Are Compression Socks Good For Jogger’s Heel?
Compression socks can offer relief for some individuals with plantar fasciitis by improving blood circulation and reducing swelling. The compression helps support the foot’s arch and may alleviate pain. However, results vary, and it’s crucial to ensure proper sizing and consult with a healthcare professional for personalized recommendations. While compression socks can be a helpful component of a treatment plan, they are not a standalone solution. Further interventions may be necessary in addition to compression socks for effective plantar fasciitis management.
Who Usually Gets Plantar Fasciitis?
Plantar fasciitis commonly affects individuals who engage in activities that place excessive stress on the feet. This group includes but is not limited to runners, athletes, and those with occupations requiring prolonged standing. People between 40 and 60 years old are more susceptible to plantar fasciitis. Factors like obesity, high-impact sports, improper footwear, and certain foot conditions increase the risk. Additionally, individuals with high or low arches and tight Achilles tendons may be predisposed. Genetics, biomechanics, and lifestyle contribute to varying degrees in plantar fasciitis development.
Why is Plantar Fasciitis so Hard to Heal?
This condition can be challenging to heal due to several factors. The plantar fascia, a thick band of tissue, undergoes repetitive stress, leading to microtears and inflammation. Limited blood supply to the area slows down the healing process. Ignoring symptoms, inadequate rest, and persistent strain can exacerbate the condition. Additionally, individual variations in foot structure, biomechanics, and contributing factors like obesity can complicate recovery.
Learn More About Alternative Ways to Alleviate Your Pain
Get back to doing the things you love, faster & without surgery.
Request an Appointment Today!
Sources:
[1] Kalia, R. B., Singh, V., Chowdhury, N., Jain, A., Singh, S., & Das, L. (2020). Role of platelet rich plasma in chronic plantar fasciitis: a prospective study. Indian Journal of Orthopaedics, 55(S1), 142–148. https://doi.org/10.1007/s43465-020-00261-w
[2] Naik, S., Agarwal, S., Prakash, S., Bhandari, R., & Agrawal, P. V. (2021). Autologous PRP injection: A safe solution for plantar fasciitis. Journal of Arthroscopy and Joint Surgery, 8(3), 253–255. https://doi.org/10.1016/j.jajs.2020.12.003