Chronic hip pain, a prevalent and often debilitating condition, casts a shadow over the lives of countless individuals. Afflicting people of various ages and backgrounds, chronic hip pain manifests in persistent discomfort, restricting daily activities and diminishing overall quality of life. Stemming from diverse sources such as osteoarthritis, bursitis, tendinitis, and other underlying disorders or injuries, this condition demands comprehensive understanding and targeted interventions. Amidst the quest for effective treatments, Platelet-Rich Plasma (PRP) therapy has emerged as a promising alternative, offering hope for natural healing and improved functionality. As individuals grapple with the challenges posed by chronic hip pain, exploring its origins, symptoms, and the revolutionary potential of PRP therapy becomes pivotal for fostering effective pain management and enhancing well-being.
Understanding Chronic Hip Pain:
Chronic hip pain can originate from an array of sources, including osteoarthritis, bursitis, tendinitis, and other disorders or injuries affecting the hip joint. Osteoarthritis, the gradual wear and tear of joint surfaces, often leads to pain, inflammation, and reduced mobility. Bursitis involves inflammation of the bursae, small fluid-filled sacs that cushion the joints, while tendinitis refers to inflammation of the tendons surrounding the hip joint. Both bursitis and tendonitis can contribute to chronic hip pain. Disorders such as hip dysplasia, labral tears, or traumatic injuries may also contribute to persistent hip pain, making a detailed diagnosis crucial for effective treatment.
Anatomy of The Hip Joint:
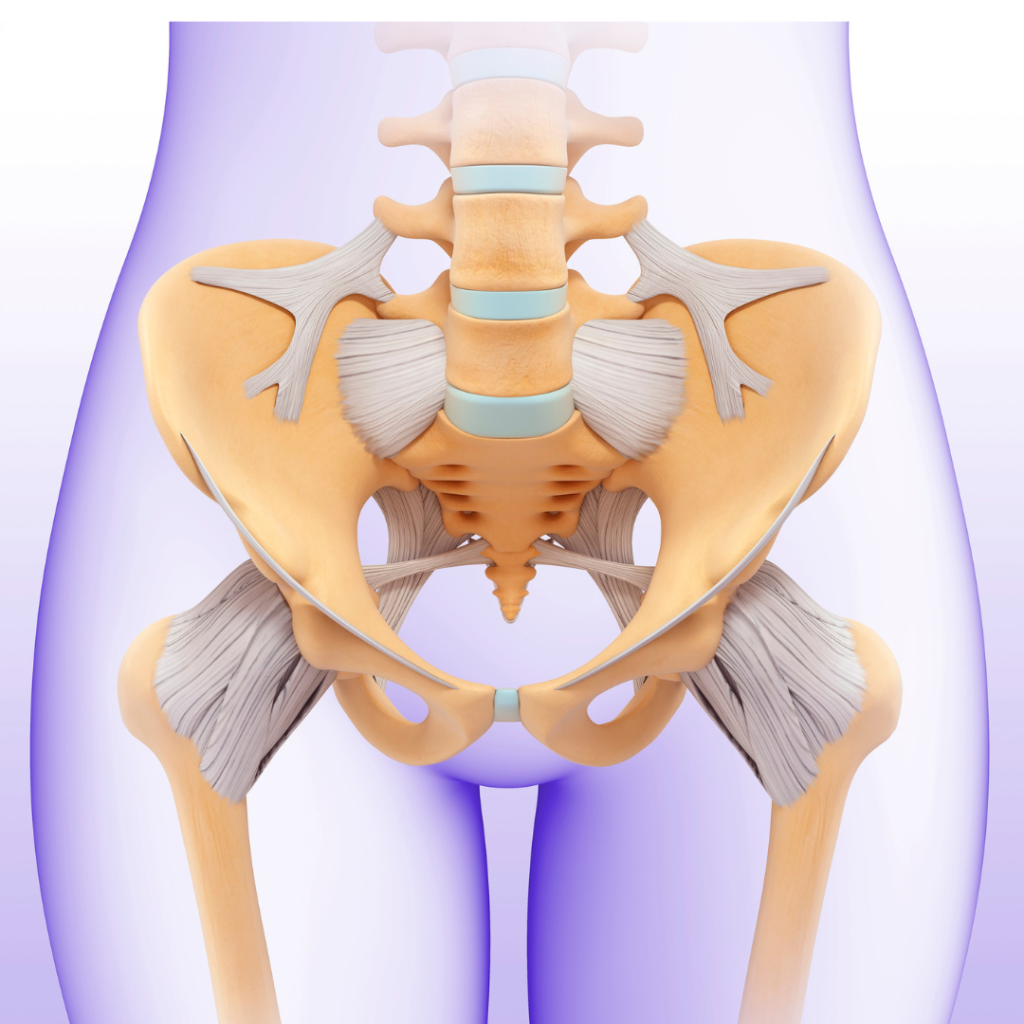
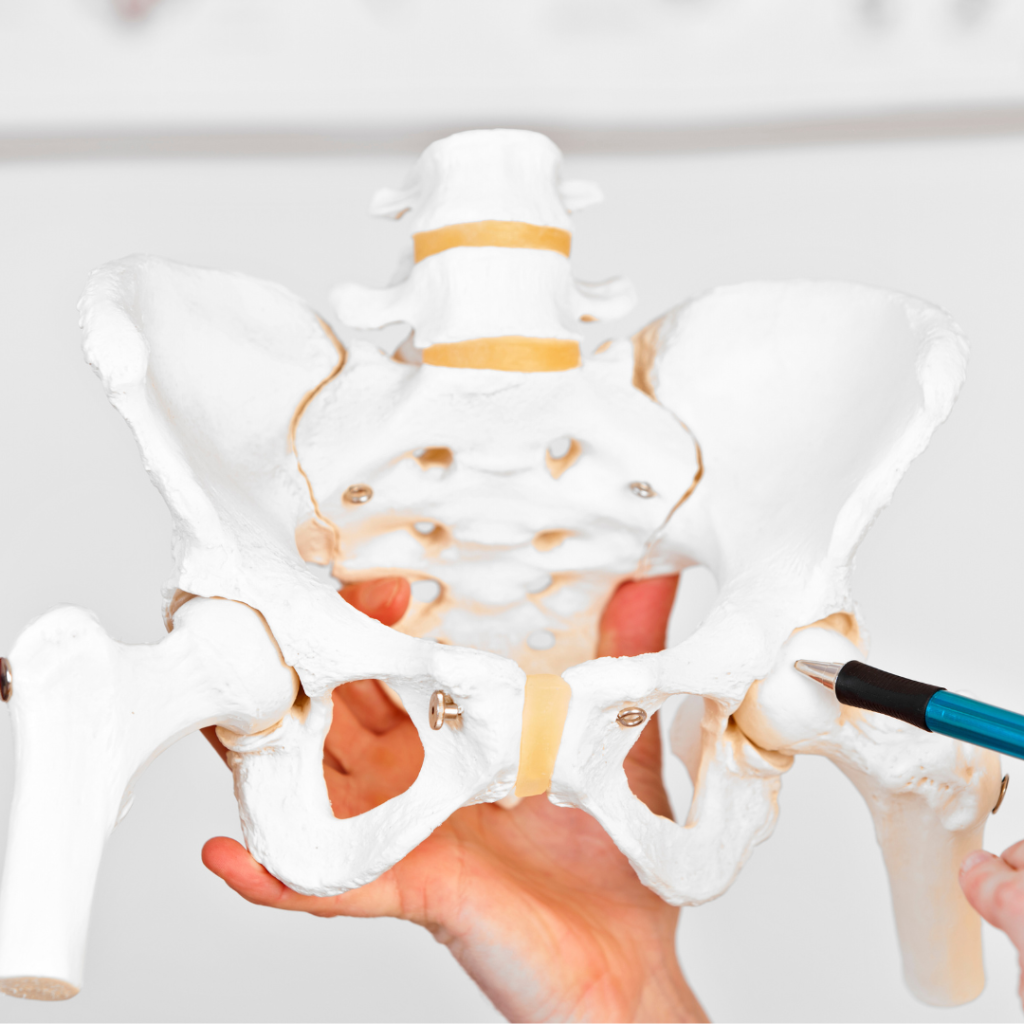
Understanding the anatomy of the hip joint is fundamental to grasp the complexities associated with chronic hip pain and the potential effectiveness of treatments like Platelet-Rich Plasma (PRP) therapy. The hip joint is a marvel of biomechanical engineering, comprising bones, ligaments, tendons, and muscles working in harmony.
What is the Hip Joint Made up of?
Bones: The hip joint involves the collaboration of two major bones: the femur (thigh bone) and the acetabulum (a concave socket in the pelvic bone). This ball-and-socket arrangement allows for a wide range of motion.
Articular Cartilage: Articular cartilage coats the surfaces of the femoral head and the acetabulum. This type of cartilage is a smooth and slippery tissue that facilitates seamless movement within the joint. This cartilage acts as a cushion, reducing friction and absorbing shock during activities.
Synovial Membrane: The synovial membrane lines the inside of the hip joint and produces synovial fluid. This fluid lubricates the joint, nourishes the articular cartilage, and ensures smooth, pain-free motion.
Ligaments: Ligaments are sturdy bands of connective tissue that connect bones to provide stability. In the hip joint, ligaments such as the iliofemoral, ischiofemoral, and pubofemoral ligaments play crucial roles in supporting the joint’s integrity.
Tendons: Tendons connect muscles to bones, facilitating movement. The tendons around the hip, including the powerful iliopsoas and the gluteal tendons, contribute to the joint’s function and stability.
Muscles: A complex network of muscles surrounds the hip joint, enabling various movements like flexion, extension, abduction, adduction, and rotation. The hip abductors, hip flexors, and gluteal muscles are key players in maintaining balance and functionality.
Bursae: Bursae are small, fluid-filled sacs situated around the hip joint. They act as cushions, reducing friction between bones, tendons, and muscles. Bursae play a crucial role in preventing irritation and inflammation during movement.
Understanding the intricacies of the hip joint lays the foundation for comprehending the potential sources of chronic hip pain. Conditions like osteoarthritis, bursitis, tendinitis, or injuries to any of these components can disrupt the harmonious function of the hip joint, leading to discomfort and limited mobility.
Where Do You Feel Hip Pain?
The hip joint, one of the largest in the body, is a pivotal hub for movement, weight-bearing, and balance. The spectrum of hip pain can vary, ranging from a temporary inconvenience to a more complex issue requiring medical attention. The precise location of the pain often provides valuable clues about the underlying problem within the hip joint.
Hip Pain that Feels:
Surface-level- may indicate issues with muscles, tendons, or ligaments.
Deep within hip- might signal that there are problems within the bones or cartilage.
Radiates to back or Groin- may stem from issues like sciatica, hip bursitis, osteoarthritis, labral tears, muscle strain, herniated discs, or pelvic conditions.

The nature of hip pain can be diverse, presenting as intermittent discomfort that may exacerbate during movement and improve with rest. Some individuals experience fluctuations in pain levels throughout the day, with heightened sensations in the morning or even at night, particularly if sleeping on the side corresponding to the affected hip.
Managing hip pain at home typically involves temporary cessation of physical activities and the use of over-the-counter pain relievers. However, seeking professional medical advice becomes crucial when hip pain significantly disrupts daily routines or persists beyond a few days without improvement. A healthcare provider can conduct a thorough evaluation, identify the root cause of the pain, and recommend appropriate interventions tailored to the individual’s specific condition.
Disorders and Injuries that Contribute to Chronic Hip Pain
Understanding and addressing these contributing factors are essential for effective prevention and treatment:
Osteoarthritis: Gradual wear and tear of joint surfaces leading to pain, inflammation, and reduced mobility.
Bursitis: Inflammation of the bursae, small fluid-filled sacs that cushion the joints, causing pain and swelling.
Tendinitis: Inflammation of the tendons surrounding the hip joint, resulting in pain and restricted movement.
Hip Dysplasia: An abnormal formation of the hip joint that can lead to joint instability, pain, and early arthritis.
Labral Tears: Tears in the cartilage (labrum) surrounding the hip joint, often causing pain and discomfort.
Traumatic Injuries: Fractures, dislocations, or other injuries resulting from accidents or trauma, contributing to chronic hip pain.
PRP Therapy for Chronic Hip Pain:
Platelet-Rich Plasma (PRP) therapy stands as a beacon of hope for individuals grappling with chronic hip pain, offering a range of potential benefits that extend beyond conventional treatment options.
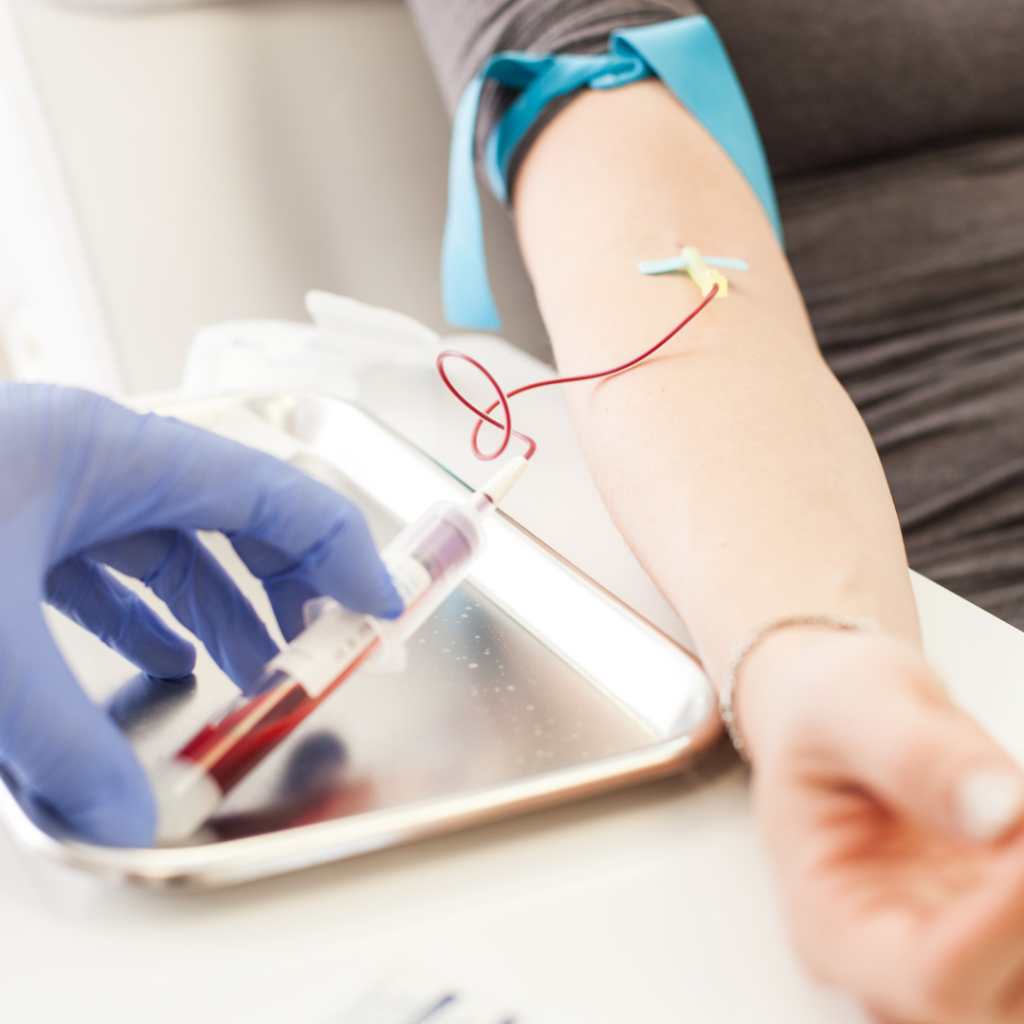
Platelet-Rich Plasma (PRP) therapy involves extracting a patient’s blood, concentrating platelets, and injecting the resulting PRP into the affected area, promoting natural healing processes and reducing inflammation.
Benefits of PRP for Chronic Hip Pain
- Natural Healing Mechanisms: PRP therapy harnesses the body’s natural healing mechanisms. By concentrating platelets and growth factors found in the patient’s own blood, the treatment stimulates and accelerates the innate healing processes within the hip joint. This natural approach promotes tissue regeneration, aiding in the repair of damaged structures.
- Reduced Hip Pain: One of the primary objectives of PRP therapy is to alleviate pain associated with chronic hip conditions. The concentrated platelets release growth factors that target inflammation, offering relief from pain and discomfort.
- Improved Hip Functionality: Beyond pain relief, PRP therapy aims to enhance joint functionality. The growth factors released during the healing process contribute to the restoration of damaged tissues, improving the overall function of the hip joint. This may include, increased range of motion and improved joint stability.
- Minimized Recovery Time: PRP therapy is known for its potential to expedite the healing process. By jumpstarting the body’s natural repair mechanisms, the treatment may lead to a faster recovery compared to some traditional interventions. Reduced downtime enables individuals to resume their regular activities sooner, minimizing the impact of chronic hip pain on their daily lives.
- Minimized Allergic Reactions: Physicians collect PRP from the patient’s own blood. Therefore, the risk of allergic reactions is minimal. This makes PRP therapy a safer option for individuals who may be sensitive to certain medications or foreign substances.
- Versatility Across Conditions: PRP therapy exhibits versatility in addressing various chronic hip conditions, including osteoarthritis, bursitis, tendinitis, hip dysplasia, labral tears, and other injuries. Its adaptability makes it a viable option for a diverse range of patients, providing a comprehensive and holistic approach to managing chronic hip pain.
Am I a Good Candidate for PRP Therapy?
If you have been living with chronic hip pain and are looking for relief, you may be a suitable candidate for PRP therapy. Evaluation criteria, patient suitability, and individual considerations play a crucial role in determining the effectiveness of this treatment. Understanding the multitude of benefits that PRP therapy brings to the table enhances the appeal of this innovative treatment for those seeking relief from chronic hip pain. While the decision to pursue PRP therapy should be made in consultation with healthcare professionals, the potential for natural healing, pain reduction, improved functionality positions PRP therapy as a promising alternative in the world of hip pain management.
Evaluation Criteria for PRP Therapy:
Severity of Chronic Hip Pain: Physicians consider PRP therapy for individuals with moderate to severe chronic hip pain that doesn’t respond well to conventional treatments. The level of pain and its impact on daily activities are crucial factors in evaluating the need for PRP.
Underlying Condition: The specific cause of chronic hip pain plays a significant role in determining candidacy. Conditions such as osteoarthritis, bursitis, and tendinitis are often considered suitable for PRP therapy, but the appropriateness may vary based on individual circumstances.
Overall Health Status: The general health of the patient is a key consideration. Individuals with chronic health conditions or compromised immune systems may need careful assessment to ensure that PRP therapy is a safe and viable option.

Patient Suitability and Considerations:
Previous Treatment Responses: Individuals who have not experienced significant relief from conservative treatments like medications, physical therapy, or lifestyle modifications may be consider PRP therapy. This therapy is often seen as an option when other interventions do not provide the desired results.
Medical History and Allergies: A thorough review of the patient’s medical history is essential to identify any potential contraindications or allergies that could affect the safety and effectiveness of PRP therapy.
Consultation with Healthcare Professionals: Ultimately, the decision for PRP therapy candidacy should be made in consultation with healthcare professionals. Orthopedic specialists or pain management experts can assess the individual’s specific case, taking into account all relevant factors to determine whether PRP therapy is a suitable option.
What Does a PRP Appointment Look Like?
First Steps:
Consultation: The first step is a consultation with a healthcare professional, often a doctor or specialist. During this discussion, the patient’s medical history, symptoms, and previous treatments are reviewed to determine if PRP therapy is a suitable option.
Diagnosis and Evaluation: Fisrt, the healthcare provider may conduct a physical examination. If necessary, imaging tests to diagnose the specific hip condition may be ordered. This step helps in tailoring the PRP treatment plan to the individual’s needs.
Informed Consent: Before the PRP procedure, the healthcare provider explains the treatment, potential benefits, and any associated risks. The patient is provided with information and an opportunity to ask questions, and informed consent is obtained.
Day of Appointment:
Blood Collection: On the day of the PRP appointment, a small amount of the patient’s blood is drawn. The blood is typically from the arm, similar to a routine blood test.
Centrifugation: The collected blood is then placed in a centrifuge, a machine that spins rapidly to separate its components. This process isolates and concentrates the platelets and growth factors from the blood plasma.
PRP Preparation: After centrifugation, the physician prepares the concentrated PRP. The resulting PRP solution, rich in platelets and growth factors, is what physicians will inject during the therapy.
Local Anesthesia Injection (if needed): Together, the physician and patient will decide if a local anesthetic will be applied to the hip area. Local anesthetic is used to minimize discomfort during the injection.
PRP Injection: The physician injects the prepared PRP directly into the affected hip joint or the area experiencing chronic pain. The PRP injection is typically guided by imaging techniques such as ultrasound to ensure precision.
Observation and Recovery: After the PRP injection, physicians may observe the patient for a short period. Occasionally, some providers may recommend a brief period of rest or limitation of certain activities immediately following the procedure.
After The Injection:
Post-Procedure Instructions: Patients receive specific instructions for post-procedure care. These may include avoiding strenuous activities for a short period and managing any temporary discomfort at the injection site.
Follow-Up: Depending on the healthcare provider’s protocol, a follow-up appointment may be scheduled. The follow up serves to monitor progress, assess the response to PRP therapy, and make any necessary adjustments to the treatment plan.
Seeking Professional Advice
It’s important to note, the details of a PRP appointment can vary based on the healthcare provider’s practices and the specific needs of the patient. Always consult with a qualified healthcare professional for personalized information and guidance.
Conclusion
In summary, Platelet-Rich Plasma (PRP) therapy emerges as a solution for those wrestling with the challenges of chronic hip pain. It offers a ray of hope for enhanced well-being and functionality. By delving into the various origins of chronic hip pain, individuals gain the knowledge needed to navigate their treatment journey. The benefits of PRP therapy span from capitalizing on the body’s natural healing mechanisms to reducing pain. Additionally, PRP may also improve joint functionality. This personalized approach not only accelerates the healing process, but also minimizes recovery time. PRP can allow individuals to swiftly reclaim their daily lives.
FAQs For Chronic Hip Pain
How do you Treat Chronic Hip Pain?
Physicians effectively treat chronic hip pain through various approaches tailored to the specific cause. Conservative measures include physical therapy, pain medications, and lifestyle modifications. In cases where these prove insufficient, advanced interventions like Platelet-Rich Plasma (PRP) therapy emerge as a promising option. PRP therapy can stimulate the natural healing process and help to alleviate pain and restore function.
Why do I Have Hip Pain All The Time?
Persistent hip pain can result from various underlying factors such as osteoarthritis, bursitis, tendinitis, or structural issues like labral tears. Inflammatory conditions, overuse, injury, or degeneration may contribute. Lifestyle factors, age, and genetics can also play a role. Identifying the specific cause through a medical evaluation is crucial for effective treatment.
Is Walking Good for Hip Pain?
Yes, walking can be beneficial for hip pain as it promotes joint flexibility, strength, and overall well-being. However, it’s crucial to consider the cause of hip pain. In conditions like osteoarthritis, gentle walking is often recommended. For acute injuries or severe pain, consulting with a healthcare professional is advised. They can provide personalized guidance on the appropriate level of activity, ensuring walking supports hip health without exacerbating underlying issues.
What is the Best Sleeping Position for Hip Pain?
For hip pain relief during sleep, the best position is usually lying on your back with a pillow supporting your knees. This aligns the spine and reduces pressure on the hips. Alternatively, lying on the side with a pillow between the knees can also alleviate hip pain by maintaining proper alignment. Experiment with positions to find what suits you best. Consider consulting with a healthcare professional for personalized advice based on the specific cause of your hip pain.
Can You Fix a Bad Hip Without Surgery?
Yes, non-surgical interventions can effectively address hip issues. Physical therapy, targeted exercises, lifestyle modifications, and medications may alleviate symptoms and improve hip function. In some cases, innovative treatments like Platelet-Rich Plasma (PRP) therapy can stimulate natural healing processes. However, the effectiveness depends on the specific condition.
What is The Average Age for Hip Replacement?
The average age for hip replacement surgery typically ranges from 50 to 80 years old. While it’s more common in older adults, hip replacements can be performed on younger individuals with certain conditions. However, it’s important to note that an individual’s lifespan may limit the number of hip replacements they can get. This is because the artificial joint may have a lifespan of approximately 15 to 20 years. Multiple replacements in a lifetime pose challenges, making careful consideration essential.
Learn More About Alternative Ways to Alleviate Your Pain
Get back to doing the things you love, faster & without surgery.
Request an Appointment Today!
Sources:
[1] Ortiz-Declet, V., Iacobelli, D. A., Battaglia, M. R., Go, C. C., Maldonado, D. R., Lall, A. C., & Domb, B. G. (2020). The effect of platelet-rich plasma in patients with early hip osteoarthritis: a pilot study. Journal of Hip Preservation Surgery, 7(3), 496–502. https://doi.org/10.1093/jhps/hnaa044